Table of Contents
Cholesterol is a waxy, fat-like substance found in your blood. While your body needs cholesterol’s to build healthy cells, having high levels of cholesterol can increase your risk of heart disease. Cholesterol’s is carried through your bloodstream by carriers made of fat (lipid) and proteins. These carriers are called lipoproteins. There are two types of cholesterol’s: low-density lipoprotein (LDL), often referred to as “bad” cholesterol, and high-density lipoprotein (HDL), known as “good” cholesterol’s.
High levels of LDL cholesterol’s can lead to several adverse health effects, primarily increasing the risk of cardiovascular diseases. In this article, we’ll delve into the potential consequences of high LDL cholesterol’s, how it affects your body, and what you can do to manage and lower your cholestero’s levels effectively.
The Role of LDL Cholesterol
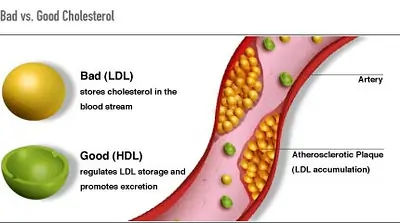
Before exploring the dangers of high LDL cholesterol’s, it’s important to understand its role in the body. LDL cholesterol’s is responsible for transporting cholesterol’s to cells throughout your body, where it’s used for various functions, such as building cell membranes and producing hormones. However, when there is too much LDL cholesterol’s in the blood, it can lead to health problems.
Consequences of High LDL Cholesterol
1. Atherosclerosis
- Plaque Formation: High levels of LDL cholesterol’s contribute to the buildup of plaques in the arteries, a condition known as atherosclerosis. These plaques are composed of cholesterol, fatty substances, cellular waste products, calcium, and fibrin.
- Arterial Narrowing: Over time, these plaques can harden and narrow the arteries, restricting blood flow to vital organs and tissues. This reduced blood flow can cause a variety of symptoms and complications.
2. Heart Disease
- Coronary Artery Disease (CAD): The restricted blood flow caused by atherosclerosis can lead to coronary artery disease. This condition occurs when the coronary arteries, which supply blood to the heart muscle, become narrowed or blocked.
- Angina: One of the symptoms of CAD is angina, which is chest pain or discomfort due to reduced blood flow to the heart muscle.
- Heart Attack: If a plaque ruptures, a blood clot can form, blocking blood flow to a part of the heart, causing a heart attack (myocardial infarction).
3. Stroke
- Carotid Arteries: Similar to heart disease, if plaques form in the arteries leading to the brain (carotid arteries), they can reduce or block blood flow to parts of the brain.
- Ischemic Stroke: A stroke can occur if the blood supply to part of the brain is significantly reduced or blocked, leading to the death of brain cells.
- Transient Ischemic Attack (TIA): Also known as a mini-stroke, a TIA is a temporary blockage of blood flow to the brain, causing stroke-like symptoms that usually resolve within 24 hours but signal a high risk of a future stroke.
4. Peripheral Artery Disease (PAD)
- Reduced Blood Flow to Limbs: High LDL levels can also lead to atherosclerosis in the arteries that supply blood to the limbs, a condition known as peripheral artery disease.
- Pain and Cramping: This can cause pain and cramping in the legs and hips, especially during physical activity (claudication).
- Critical Limb Ischemia: In severe cases, PAD can lead to critical limb ischemia, where reduced blood flow causes severe pain and sores or infections in the legs and feet.
5. Chronic Kidney Disease
- Renal Arteries: The kidneys rely on healthy blood vessels to filter waste from the blood. Atherosclerosis in the renal arteries can lead to chronic kidney disease by reducing blood flow to the kidneys.
- Kidney Function Impairment: This impairs their function over time, potentially leading to kidney failure if left untreated.
6. Reduced Blood Flow
- Poor Circulation: In general, high LDL cholesterol’s can cause reduced blood flow throughout the body, affecting various organs and tissues.
- Wound Healing: Poor circulation can lead to symptoms such as poor wound healing and increased risk of infections, especially in the extremities.
7. Inflammation
- Arterial Inflammation: High LDL cholesterol’s can also promote inflammation within the arteries, further contributing to the development and progression of atherosclerosis.
- Plaque Rupture: Chronic inflammation is a key factor in the rupture of atherosclerotic plaques, which can precipitate heart attacks and strokes.
ALSO READ: Need to Know About the Flu: Why Is Flu So Dangerous?
Prevention and Management of High LDL Cholesterol
Managing high LDL cholesterol’s typically involves a combination of lifestyle changes and, in some cases, medication. Here are some effective strategies to lower LDL cholesterol’s:
Dietary Changes
- Heart-Healthy Diet: Adopting a heart-healthy diet can significantly reduce LDL cholesterol’s levels. This diet should be low in saturated and trans fats and high in fruits, vegetables, whole grains, and healthy fats (such as those found in olive oil, nuts, and avocados).
- Fiber Intake: Increasing soluble fiber intake (found in oats, beans, lentils, fruits, and vegetables) can help lower cholesterol by binding to it in the digestive system and removing it from the body.
- Reduce Sugar and Refined Carbohydrates: Limiting sugar and refined carbohydrates can also help improve cholesterol levels and overall cardiovascular health.
Exercise
- Regular Physical Activity: Engaging in regular physical activity, such as brisk walking, running, cycling, or swimming, can help raise good cholesterol’s (HDL) and lower bad cholesterol’s (LDL).
- Exercise Recommendations: Aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity aerobic exercise per week, along with muscle-strengthening activities on two or more days per week.
Weight Management
- Healthy Weight: Maintaining a healthy weight is crucial for managing cholesterol levels. Excess body weight can contribute to higher LDL levels and lower HDL levels.
- Weight Loss: If you are overweight, losing even a small percentage of your body weight (5-10%) can significantly improve your cholesterol’s profile.
Smoking Cessation
- Quit Smoking: Smoking lowers good cholesterol’s (HDL) and increases the risk of heart disease. Quitting smoking can improve your HDL levels and overall cardiovascular health.
Medications
- Statins: Statins are the most commonly prescribed medications for lowering LDL cholesterol’s. They work by blocking a substance your body needs to produce cholesterol and can help reduce the risk of heart attacks and strokes.
- Other Medications: Other cholesterol-lowering medications include bile acid sequestrants, cholesterol’s absorption inhibitors, and PCSK9 inhibitors. Your doctor will determine the best medication based on your specific health needs and risk factors.
Regular Monitoring
- Cholesterol Testing: Regular monitoring of cholesterol’s levels and cardiovascular health is crucial for early detection and management of high LDL cholesterol’s. Your doctor may recommend more frequent testing if you have a history of high cholesterol’s or other risk factors for heart disease.
- Risk Assessment: In addition to cholesterol’s levels, your doctor will consider other factors such as age, family history, smoking status, blood pressure, and presence of diabetes to assess your overall risk of cardiovascular disease.
1. What is LDL cholesterol and why is it considered “bad”?
LDL stands for low-density lipoprotein, a type of cholesterol that transports cholesterol’s from the liver to the cells. It is considered “bad” because high levels of LDL cholesterol’s can lead to the buildup of plaques in the arteries, causing atherosclerosis. This condition can narrow and harden the arteries, increasing the risk of heart disease, heart attacks, and strokes.
2. What are the symptoms of high LDL cholesterol’s?
High LDL cholesterol’s typically does not cause any symptoms on its own. It is often discovered through a blood test called a lipid panel. However, complications arising from high LDL cholesterol’s, such as atherosclerosis, can lead to symptoms like chest pain (angina), shortness of breath, pain in the legs or feet, or stroke-like symptoms. Regular screening is essential for early detection and management.
3. How can I lower my LDL cholesterol’s levels naturally?
Diet: Eat a heart-healthy diet rich in fruits, vegetables, whole grains, and healthy fats. Avoid foods high in saturated and trans fats.
Exercise: Engage in regular physical activity, aiming for at least 150 minutes of moderate-intensity exercise per week.
Weight Management: Maintain a healthy weight or lose weight if you are overweight.
Quit Smoking: If you smoke, seek help to quit, as smoking can lower good cholesterol and increase the risk of heart disease.
4. What medications are available to lower LDL cholesterol’s?
Statins: These are the most commonly prescribed and work by reducing the amount of cholesterol produced by the liver.
Bile Acid Sequestrants: These medications help remove cholesterol’s from the blood by binding to bile acids.
Cholesterol Absorption Inhibitors: These reduce the absorption of cholesterol’s from the diet.
PCSK9 Inhibitors: These are injectable medications that help the liver absorb more LDL cholesterol, lowering the levels in the blood.
Your doctor will determine the best medication based on your individual health needs and risk factors.
5. How often should I get my cholesterol’s levels checked?
Adults: It is recommended to have a cholesterol’s test every 4-6 years if you are at low risk for heart disease.
Individuals at higher risk: Those with risk factors such as a family history of heart disease, high blood pressure, diabetes, or being overweight may need more frequent testing.
People already diagnosed with high cholesterol: Regular monitoring as advised by your healthcare provider is crucial to manage and adjust treatment plans effectively.
Consult with your doctor to determine the appropriate testing schedule for your specific situation.
Conclusion
High LDL cholesterol’s is a significant risk factor for various cardiovascular diseases, including heart disease, stroke, and peripheral artery disease. Understanding the consequences of high LDL cholesterol’s and taking proactive steps to manage and lower your cholesterol levels can significantly reduce your risk of these serious health conditions.
By adopting a heart-healthy lifestyle, including a balanced diet, regular exercise, maintaining a healthy weight, quitting smoking, and following your doctor’s recommendations for medications and monitoring, you can keep your cholesterol’s levels in check and protect your cardiovascular health. Regular check-ups and open communication with your healthcare provider are essential in managing your cholesterol’s and overall health effectively.



